The Tar Heel State earned failing marks for healthcare and its costs according to a list by Forbes Advisor ranking of all 50 states.
North Carolina was ranked as the third worst state for healthcare and the worst state in the country for healthcare costs.
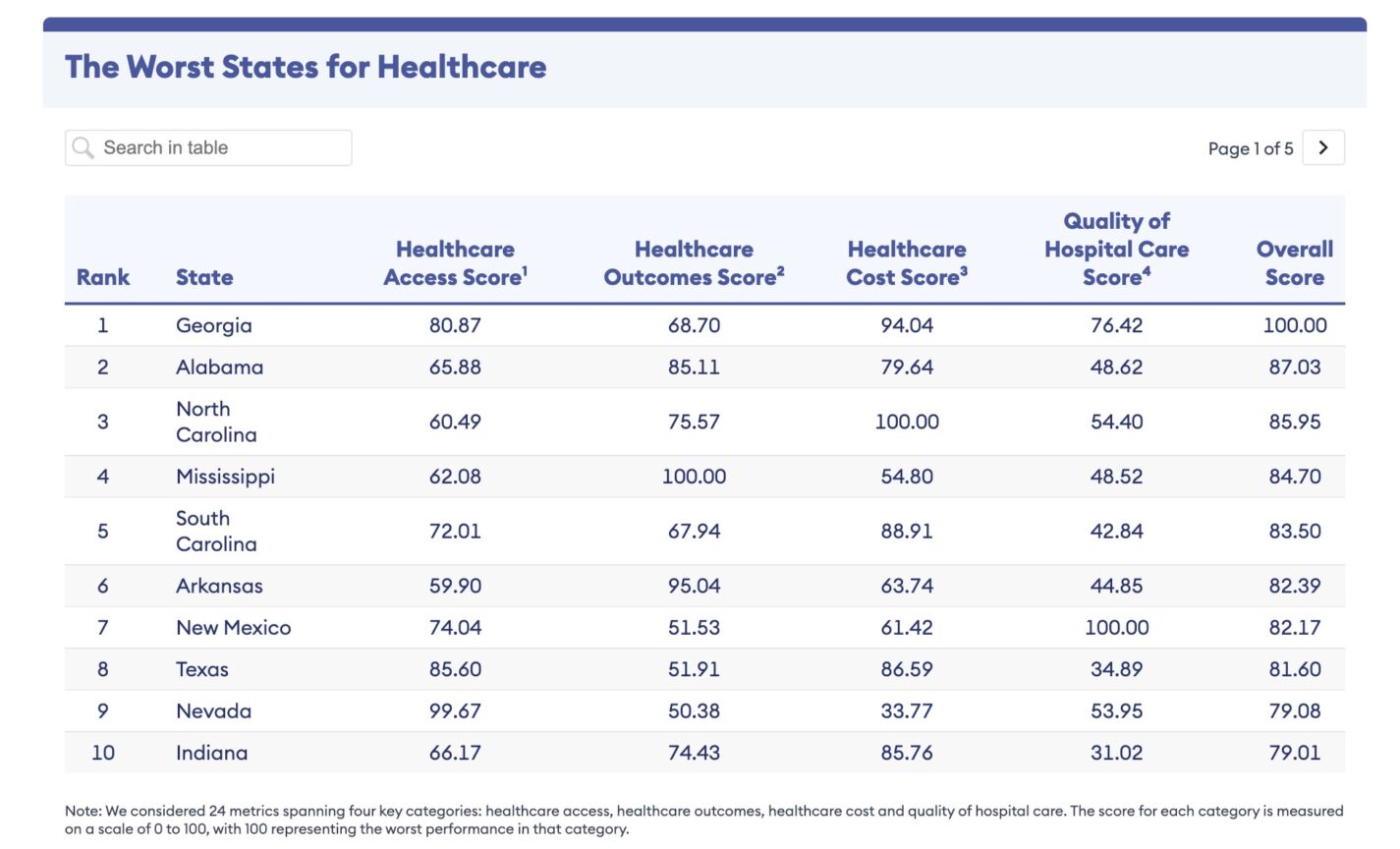
Forbes Advisor compared all 50 states across 24 metrics spanning four key categories: healthcare access, healthcare outcomes, healthcare cost, and quality of hospital care.
The Forbes article mentions that according to a recent Harris Poll, more than 70% of adults say the healthcare system is failing to meet their needs in at least one way.
When it comes to healthcare costs, North Carolinians with single health insurance coverage through an employer pay the eighth highest premium nationwide, $1,847 annually.
Employers in the state cover the eighth lowest percentage of employees’ annual health insurance premiums on average, 76.18% for employees with single coverage.
This isn’t the first time healthcare costs have been questioned in the state. Last month, hospitals were called out in a report from State Treasurer Dale Folwell’s office that showed a wide range in hospital pricing, huge price markups from Medicare rates, and a lack of price transparency.
Researchers from the NC State Health Plan for Teachers and State Employees investigated hospital prices and compliance with federal price transparency rules across 16 common shoppable services at 140 hospitals. Researchers from the Johns Hopkins Bloomberg School provided data analysis based on June 2023 data from Turquoise Health, a software company that collects and displays hospital prices for patients and researchers to facilitate price transparency in health care.
In terms of hospital pricing, North Carolina hospitals levy massive price markups of up to 1,120% on routine care and basic services, with the most expensive subset of hospitals charging commercially insured patients as much as 1,670% more than other hospitals for the same service, which could cost patients and businesses tens of thousands of dollars.
The report found that when it came to Medicare rates, some North Carolina hospitals charge commercially insured patients more than 700% of Medicare rates for some common shoppable services, like a urinalysis test, which can carry a 1,120% median markup from Medicare, forcing patients to pay a median $28.80, while Medicare pays a median of just $2.36.
A previously published report indicates that inflated prices are unnecessary, given that most North Carolina hospitals self-reported profiting off Medicare rates over six years.
In its article, Forbes also found that the state also has the:
- Fifth lowest number of nurse practitioners, 4.28 per 10,000 state residents.
- Eighth highest infant mortality rate, 6.76 deaths per 1,000 live births.
- Ninth highest rate of both stroke deaths, 44.13 per 100,000 state residents, and influenza and pneumonia deaths 13.40 per 100,000 state residents.
North Carolina has 13.45 primary care physicians available per 10,000 residents.
Minnesota ranked as the best state overall for healthcare, followed by Massachusetts, Rhode Island, Connecticut, Vermont, New Hampshire, Michigan, Oregon, Maine, and Pennsylvania.
Georgia ranked the worst state overall for healthcare, followed by Alabama, North Carolina, Mississippi, South Carolina. Arkansas, New Mexico, Texas, Nevada, and Indiana.
“North Carolina has many high-quality health systems and hospitals, but often gets penalized in state rankings for healthcare because the state has not yet implemented Medicaid expansion,” a spokesperson for the North Carolina Healthcare Association (NCHA) said in an emailed statement to Carolina Journal. “Thanks to the General Assembly passing HB76 this year, that will soon change. We look forward to seeing improved rankings for the state on lists like this.”
They continued saying that the best way for individuals to stay healthy and to control their healthcare expenses is to have health coverage and to get routine preventive care, which an additional 600,000 residents will soon be able to do.
They also stressed that Southern states often rank lower on lists like this due to having comparatively higher rates of residents with chronic conditions or substance use issues affecting their health. In addition, states with large rural populations also tend to rank lower due to challenges rural community residents may have with accessing healthcare providers and transportation to medical appointments.
“The North Carolina Healthcare Association and our members are continuing with important work to recruit and retain more healthcare providers to North Carolina, to improve health in rural communities, and to eliminate racial disparities in clinical care settings,” the spokesperson said. “We are also talking with insurers to identify opportunities to make our state’s health care system work better for employers and residents. While there is clearly room for improvement, we are optimistic about the direction healthcare is heading in the state.”